'It's Cancer - Now what?'

Here’s a story we have heard too many times - You go to the doctor for a routine checkup, mammogram, or to have something looked at that seems abnormal. The doctor or radiologist decides to order a few more tests just to be safe, including a biopsy. After waiting anxiously for days or even weeks, the results arrive. It’s cancer. Finding out 'it's cancer' was the reality for nearly 2 million people across the United States in 2022 according to the CDC.
Many cancer patients and survivors describe everything after this as, ‘being in a fog,’ or ‘white noise,’ where it’s difficult or impossible to hear anything else being said after the words ‘you have cancer.’ Oncologists understand this and will usually suggest that a friend or family member also attend early appointments to take notes and provide emotional support.
Whether it is invasive ductal carcinoma, adenocarcinoma, small cell lung cancer, melanoma, cholangiocarcinoma, glioblastoma, or any of the countless other forms of cancer, the same question goes through everyone’s head:
“I’ve Just Been Diagnosed with Cancer.
Now What?”
Most do not have direct experience with cancer and know little about their specific diagnosis. Trying to understand your cancer diagnosis immediately after learning about it can be overwhelming. Patients have provided accounts of going down ‘Google rabbit holes,’ trying to learn everything there is to know about their diagnosis overnight. Others began asking friends and family what to do. These are all normal reactions.
In an effort to help incoming patients navigate this difficult time, we put together a few pieces of advice that patients and survivors said they wish they knew at the time of diagnosis. This is not meant to replace medical advice, but may offer some guidance from patients and their families who have already navigated similar challenges.
1. Seek a Second Opinion on Your Diagnosis and Treatment Options
A cancer second opinion allows patients to receive an additional review of the initial diagnosis and treatment plan, rather than relying entirely on the opinion of the doctor or facility who gave the initial diagnosis. Cancer is complex and research is continually advancing our collective knowledge. With this in mind, it is often the case that specialists and experts for a specific form of cancer may be aware of, or have access to, treatment options that might not yet be instituted in all hospitals.
A common misconception around cancer second opinions is that their sole purpose is to confirm or refine the diagnosis. While this is an important component, perhaps even more important is that oncology second opinions also confirm, modify, or refine recommended treatment options.
One patient we interviewed stated that she did not seek a second opinion after her initial breast cancer diagnosis. She told us that she thought, “I don’t need a second opinion to tell me it's cancer, they already know it's cancer?” However, after multiple surgeries and treatment complications she was able to clearly articulate exactly why, in her words, “not getting a second opinion was a big mistake. In hindsight, I wish I had a second opinion to discuss treatment options.”
In this clip, Dr. Rasmussen explains that in a cancer diagnosis, patients may also want to consider a second opinion on the pathology read, also discussed in a recent blog, 'Pathology Second Opinions - Look Again.' Watch the full webinar here.
So, where should you look for a cancer second opinion?
In the United States, start with one of the 71 National Cancer Institute (NCI) Designated Cancer Centers around the country. From within these hospitals, find a specialist in the type of cancer you have. A study from the Advisory Board surveyed over 1,200 cancer patients and found that over 52% ranked finding a “Doctor who specializes in my particular cancer” as their most important factor when choosing where to ultimately seek care.
2. Ask if Your Case Can Be Presented to a Tumor Board
A tumor board is a meeting of doctors and other healthcare professionals across various specialties at a given hospital to discuss the diagnosis and treatment options for complex cancer cases. Tumor boards, also called multidisciplinary reviews, are comprised of various individuals including but not limited to pathologists, medical oncologists, radiation oncologists, surgical oncologists, and even relevant nurses or social workers. Each member brings a different perspective to the table with the goal of creating a more holistic view of the case.
A patient we recently interviewed had his melanoma case reviewed by a tumor board. The doctors on the board had multiple opinions on a path forward. His case was then presented at a global summit of world-renowned experts in melanoma treatment and multiple opinions still remained. In the end, the patient’s surgical oncologist brought this information back to the patient and he was able to make an informed decision guided by the input of multiple doctors. What we learn from this story is that even among the top experts in the world, complex cancer cases can still have multiple paths forward in the dynamic landscape of cancer care.
One thing to note...
Tumor board review might not be available to every cancer patient since not every hospital has a tumor board and not all cases qualify for review. Typically, only complex or challenging cases reach the tumor board. This is why it is important that you ask your doctor if your hospital has a tumor board and if so, request that your case be reviewed.
3. Ask and Research if You Are a Candidate for Clinical Trials
One recent conversation with a cancer survivor stood out based on the patient’s approach to handling her initial appointments. In this case, by the time the patient had received her breast cancer diagnosis, she had already battled alongside her husband, mother, and aunt as an advocate during their cancer care journeys. She had learned during these experiences that clinical trials sometimes provide options that might be better suited for a specific form of cancer than the standard of care. So, when she received the call from her doctor saying she had breast cancer, rather than waiting for her appointment to go over treatment options, she began researching relevant clinical trials. When she arrived at her first appointment, she had a list of clinical trials she had prepared to discuss with her doctor that could potentially avoid surgery.
A common misconception is that clinical trials are only available, as one patient put it, as a “Hail Mary Pass” when all other options have been exhausted. With the advancements happening every day in cancer research, more and more clinical trials are available that can help patients avoid surgeries or offer alternative treatment plans. Some are now being conducted remotely, helping to protect patients while immunocompromised. While your participation in these trials should be discussed with your doctors and reviewed with your own personal risk calculus in mind, knowing all your alternatives beyond just the standard of care can help you find the path that is right for you.
To begin your clinical trial research, start by visiting the NIH ClinicalTrials.gov website.
4. Ask and Research What are the Cutting-Edge Treatments for Your Type of Cancer
Cancer research is dynamically changing almost daily. While the standard of care might be the appropriate path forward, it is also possible that a research hospital somewhere in the country is updating that standard with new research as you read this article. Patients are becoming more aware of this trend as a survey of 1,200 cancer patients conducted by the Advisory Board revealed that “Technology and Treatment Options” ranked as the second most important factor in choosing a hospital for treatment.
Different from clinical trials, these technologies and treatments are already fully approved and in use at leading hospitals but not yet in use at others. For instance, we interviewed a patient whose local hospital recommended surgery to remove a tumor. The patient and his wife conducted their own research and found that two leading cancer hospitals in the country were offering a new form of advanced radiation called Proton Therapy that potentially could avoid the need for surgery. The patient flew across the country to receive the treatment over a 6-month period and ultimately avoided surgery entirely which would have almost definitely caused lifelong side effects.
Another patient we interviewed had received conflicting opinions from doctors about whether to pursue a full Lymph Node Dissection (LND) to ensure his melanoma would not reoccur. Several of the doctors were against the surgery because it would likely cause lymphedema. However, one of the doctors was aware of a cutting-edge procedure known as Microscopic Lymphatic Bypass surgery that is not yet performed at many hospitals. They were able to bring in a specialist to perform this procedure successfully in conjunction with the LND, avoiding lymphedema.
In both patient’s cases, without access to these leading specialists, their treatment options would have been limited to sub-optimal outcomes. This should show that not all hospitals are created equal when it comes to cancer treatment. Seeking out experts in your specific form of cancer and understanding the most groundbreaking treatment plans can help provide options.
5. Find a Support Group for Your Specific Form of Cancer
We have learned across our interviews that cancer is hard and it can sometimes feel like you are going against it alone. Nearly every cancer survivor interviewed spoke of the value of finding a community of other cancer patients with their specific form of cancer to learn from and lean on.
These groups can sometimes be affiliated with a foundation, a cancer hospital, or completely independent. Sometimes membership in these groups requires you to be within a certain age range or within a certain geography.
These groups can be a good source of information and support from people who have been in your shoes. In this clip during a recent Purview webinar with foundations, panelists discuss how to find your community on social media and through other foundations and channels.
Watch the full webinar here.
Read more about Lisa Craine's experience and advocacy for second opinions.
6. Begin Aggregating Your Prior Medical Records
Whether you end up seeking a second opinion, applying for a clinical trial, or traveling to a leading cancer facility in search of cutting-edge technology and treatment options, you will need to begin aggregating your medical records in a single location so they are easy to share.
We know of one cancer patient who traveled from one specialty hospital to another with a literal shoebox filled with imaging CDs and a complete record of her cancer treatments. When a hospital across the country needed these records, she had to FedEx them overnight, leaving her without a copy. Fortunately, today records can be aggregated digitally to avoid this hassle and risk. Leading second opinion programs offer the ability to submit a case remotely along with all prior records, including medical imaging and pathology reports.
Today, there are tools available for patients to digitally upload, store, and share their medical records. We know that collecting records can also be difficult, but if you need help just let us know and we’d be happy to talk you through the best strategies based on our experience.
7. Don’t Forget Your Mental Health
A sometimes-overlooked area of cancer treatment is a focus on your mental health. Talking to support groups can be very helpful to find a cohort of people going through similar challenges. That said, in talking to cancer survivors and caretakers of cancer patients, numerous individuals said they wish they had contacted a therapist earlier in the process.
In one case, an individual noted that she was not ready to talk to a support group early on because that would mean “the diagnosis was real.” Another person indicated that having access to a child psychologist was immensely helpful in explaining to her kids what a cancer diagnosis meant for their family. Still, in another case, a patient shared that she still struggles with worry that her cancer will “come back metastatic” and she questions whether she has “done everything she can do.” In each of these cases, the patients indicated that having someone to talk to through these times of fear, uncertainty, and doubt has been extremely helpful and something they strongly recommended for others.
8. Seek Out Hope
A final key area raised in our patient interviews was focusing on things that bring you hope. In a recent interview, a patient and his family told the story of trying to decide which of three highly qualified specialty hospitals to choose from for treatment. His wife explained:
“We chose the hospital that gave us the most hope.”
Hope was once described to me as the ability to hold a belief for someone until they are able to hold it on their own. I think this definition holds very true in the face of a cancer diagnosis. Surround yourself with people, support groups, and hospitals that hold the beliefs that you are a powerful cancer survivor not just a patient, you have a future and not just a diagnosis and, 'you are more than just the bad things that happen to you,' even if you are too overwhelmed to hold these beliefs for yourself.
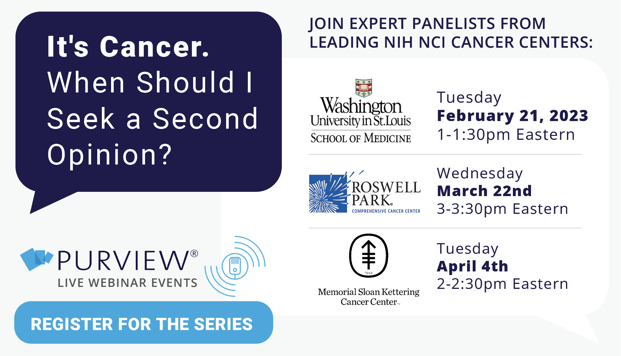
For more information and resources, register for upcoming Webinar with NIH NCI leading cancer centers: Roswell Park Cancer Center, University of Washington St. Louis Medicine, and Memorial Sloan Kettering Cancer Center: It's Cancer. When Should I Consider a Second Opinion?




